Electrocution is surprisingly common, although
rates of lightening strike are decreasing. Given that they should be well aware of the dangers of electricity, I was surprised that
electricians and people who work with electricity are most likely to be affected. Electrocutions could affect people in hospital as well as out of hospital, and as the old adage goes,
prevention is better than cure. It's not just high voltage electrocutions that cause problems, as a 33 year old with a
domestic electrocution found.
If you look hard enough, you can find plenty of information online about electrocution. The
AHA has a very thorough article online and EnlightenMe and
LITFL have cases on the
injuries associated with electrocution.
I know it's not FOAM, but the eLfH e-learning site has a fantastic e-learning module about
electrical burns. It tells you a lot about those things that you always wondered about, but weren't quite sure about, and I'd really recommend completing it if you can.
So, lets get started.
Electrocution: death as a result of exposure to electric current
Electrical injury: Tissue damage as a result of exposure to electrical current
Electrical shock: The violent response to electric current exposure often characterised by involuntary muscle contraction.
1000 people per year are estimated to die from exposure to electricity each year. In 2005, there were 11 work related electrocutions and 119 serious injuries in the workplace. Electrical injuries follow a bimodal age distribution pattern - children younger than six, and in early adulthood.
The ability of an electrical current to cause morbidity and mortality is dependent on six different factors:
- Magnitude of the current
- Voltage of the electrical source
- Resistance of tissue types involved - (bone has the most resistance)
- Duration of exposure
- Type of current
- Current pathway
There are two main types of electricity that might cause us injury - low tension and high tension.
Low Tension
- <300 Volts
- at 50hz
- Alternating current (AC)
- Domestic (110V in the US and Canada; 220V in Europe, Australia and Asia).
- Can cause VF
- Theoretical risk of late VF if shock travels through the thorax
May cause tetanic skeletal muscle contractions - stopping people from letting go from the electricity source. Because AC current is repetitive it also increases the likelihood of current flow through the heart during the relative refractory period of the cardiac cycle which can precipitate ventricular fibrillation.
- Intraoral burns are common in young children (toddlers who
explore electrical cables by placing them in their mouth). Conduction may be aided by electrolyte rich saliva. Delayed haemorrhage
is a recognised feature.
Prevention is always important, and ROSPA have lots of advice (and lots of leaflets) about how to make your home safer.
High Tension
- >1000 Volts
- Lightening strikes and overhead power cables.
- Direct current
- May cause asystole, complete heart block and QT prolongation.
- Keraunoparalysis - transient limb weakness, rarely lasting more than a few hours. Upper limbs > lower limbs.
- Lightening strikes - mortality of 30%
- extensive autonomic stimulation - hypertension, tachycardia and nonspecific electrocardiographic changes
- brain haemorrhages, oedema and nerve injury.
- Lichtenberg’s flowers
- Transient, fernlike erythematous floral pattern that develops on the skin
- Fades in 24 - 36 hours
This type of electricity simultaneously depolarises the entire
myocardium. This normally stops the heart completely, but sometimes the
heart sorts itself out again and starts working normally again (it has
intrinsic cardiac automaticity). This type of electricity also causes
thoracic muscle spasm making it very difficult to breathe. Secondary
hypoxic cardiac arreast is likely! Victims are most likely to die if they experience immediate respiratory or cardiac arrest and no treatment is provided - if treatment is provided at scene, results are often good.
DC exposure is single, and often throws the victim away. A direct strike
is uncommon, and often splashes sideways from an object or a victim may
be holding on to a struck object.
Treatment
- Early basic life support and defibrillation if needed
- Airway:
- Secure the airway early (airway burns likely)
- C-Spine Control:
- Especially if DC current - may have been ejected
- Breathing:
- AC current may paralyse thoracic muscles
- Circulation:
- Hypovolaemia from concurrent injuries likely
- ECG - assess for presence of sinus rhythm, and remember to check the QT interval
- Cannulate in a limb not involved in the current pathway
- There may be damage to vascular structures that will stop systemic circulation
- Disability:
- Look for entry and exit burns
- Cool burns as appropriate
- Remove smouldering clothes, shoes and belts.
- Exposure:
- Look for compartment syndrome (if you don't look you won't see!)
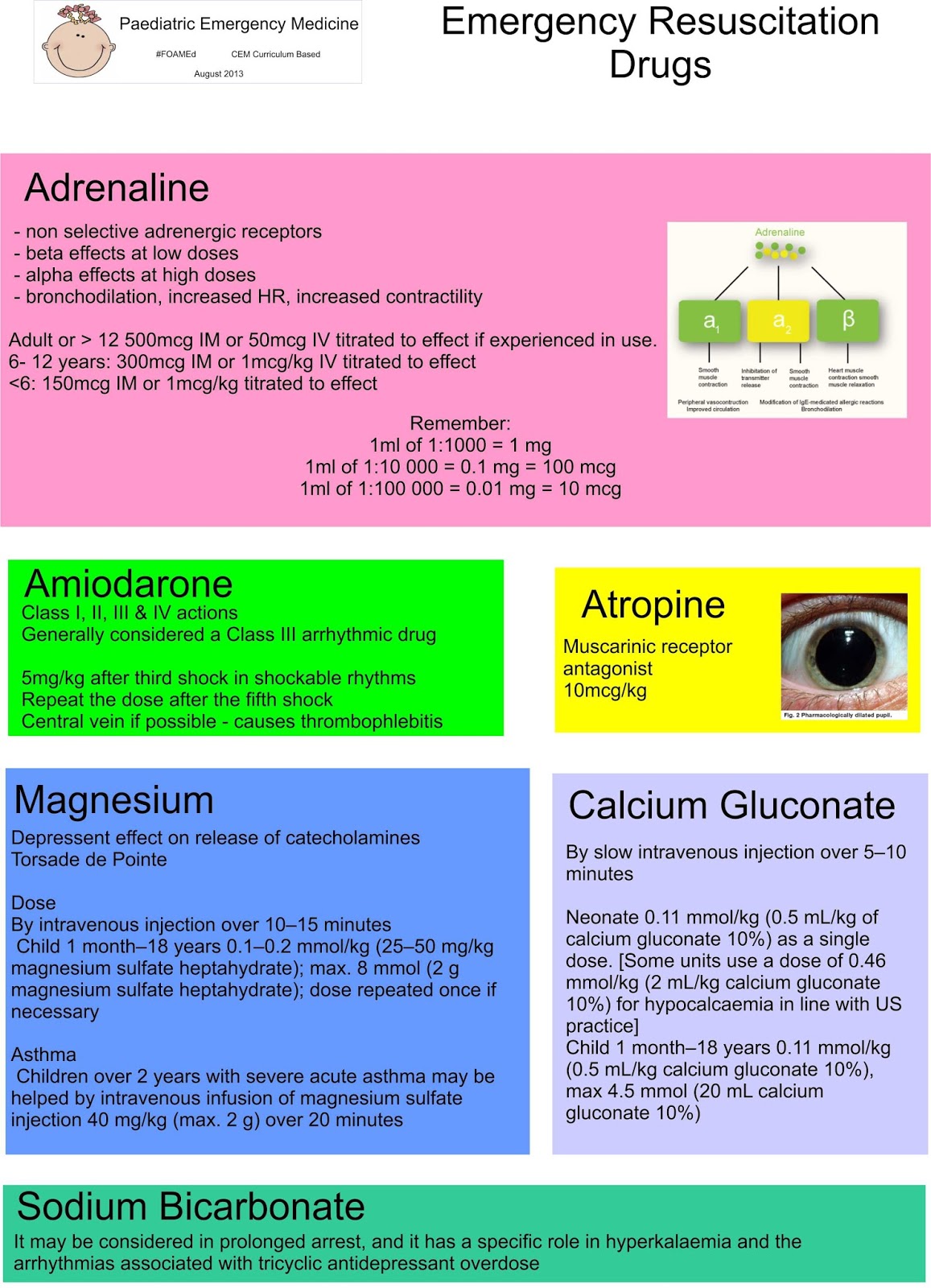
- Bloods for:
- FBC, U&E (hyperkalaemia secondary to rhabdomyolysis likely)
- Phosphate
- Calcium
- CK
- Group and Save
- Role of troponins is unclear
- Check hearing
- Risk of ruptured ear drums from lightening (Oxford Handbook of Emergency Medicine)
- Urinalysis - check for blood
- Observe
- Six hours of being asymptomatic
- Send home
- Asymptomatic patients with
- domestic and minor low voltage burns
- normal ECG
- no history suggestive of arrhythmia
- no myoglobinuria
- Admit
- Children who bite electrical flexes
- All patient with high voltage conduction injuries, or abnormalities found.
- Follow Up
- Delayed cataract formation
- Neuropsychiatric problems
- Compartment syndrome advice
The management of burns is important - we'll cover this later!