There is only one e-learning module I could find on dehydration, but as it was based on a 2010 research paper and lots has changed since then, I didn't complete the module.
EnlightenMe offers a management case on a patient with warning signs for dehydration, where appropriate action was not taken.
Causes
Worldwide the greatest number of deaths from shock probably occurs in under 5 year old children with hypovolaemia as a result of diarrhoeal illness, and gastroenteritis is still the most common cause in children.
Clinical Assessment
History
The first step to assessing the risk of dehydration is taking a full history. NICE lists many things as presentations that put people at higher risk of dehydration:
• children younger than 1 year, especially those younger than 6 months
• infants who were of low birth weight
• children who have passed six or more diarrhoeal stools in the past 24 hours
• children who have vomited three times or more in the past 24 hours
• children who have not been offered or have not been able to tolerate supplementary fluids before presentation
• infants who have stopped breastfeeding during the illness
It can be difficult to know how much fluid babies should be taking - and whether their vomiting is a result of over-feeding. Babies slowly increase their intake to 150 mls/kg and this should allow them to gain 20 – 30g weight per day.
Clinical
There is a nice poster about assessing dehydration here. I've never seen the Gorelick scale used clinically, although the concept is well known. For assessing dehydration in adults, I was taught the mnemonic "HEP B" and I think this works well in children too:
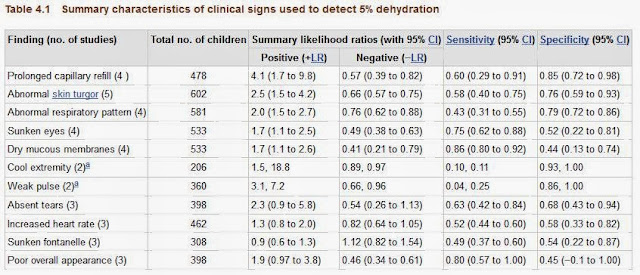
When we make our thorough assessment, we decide whether a child is clinically dehydrated or not. If we are using capillary refill we need to ensure we specify where we are checking. Worryingly, all of the standard signs that are quoted have a very low sensitivity and specificity:
 |
| NICE Guidelines: http://www.ncbi.nlm.nih.gov/books/NBK63844/pdf/TOC.pdf |

Biochemical
Do not routinely perform blood biochemical testing.Measure plasma sodium, potassium, urea, creatinine and glucose concentrations if:
- intravenous fluid therapy is required or
- there are symptoms and/or signs that suggest hypernatraemia.
Treatment
- Oral rehydration is adequate in most circumstances.
- Oral replacement fluid is best used, even in children with no signs of clinical dehydration.
- Flat fizzy drinks should not be used.
- Nasogastric rehydration can be a safe alternative to IV rehydration.
- Fluid bolus of 20ml/kg to treat clinical shock
Increase up to 40ml/kg as needed
If any more fluid than this is needed, PICU must be involved.
- Then start maintainence fluids:
1st 10kg - 100mls / kg / day
+
2nd 10kg - 50mls / kg / day
+
Then 20mls / kg / day
e.g. 25Kg = (10 x 100) + (10 x 50) + (5 x 20) = 1.6 litres
Discharge Advice
If you discharge patients home, remember to give them clear advice. The NICE guidelines on D&V are quite clear (although who knew no swimming for two weeks?).
- Continue breast feeding and other milk feeds
- Discourage use of fruit juices and fizzy drinks (until diarrhoea has stopped)
- Supplement with oral rehydration therapy as needed